Do you have these symptoms of gluten intolerance? Find out if you should be cutting out gluten from your diet STAT. Grab the PDF list of gluten intolerance symptoms so you can feel better fast.
🙋♀️What is Gluten Intolerance?
Ok first things first: what the HECK is gluten intolerance?
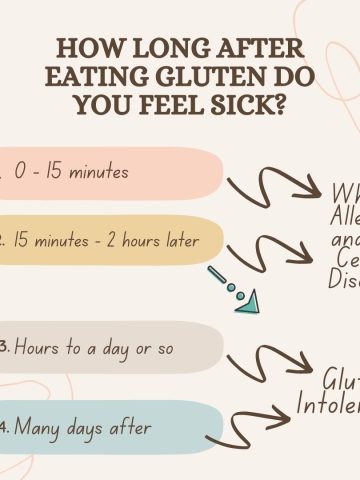
Gluten intolerance or Non-Celiac Gluten Sensitivity as it's referred to sometimes, is a condition that involves people having a "reaction" after eating gluten or gluten-containing foods.
Jump to:
- 🙋♀️What is Gluten Intolerance?
- 🍞What is gluten?
- 🗺️How common is gluten intolerance?
- ✅Signs and Symptoms of gluten intolerance
- 🙋♀️Some of the most common symptoms of gluten intolerance
- 📝Grab the Gluten Intolerance Symptom Checklist
- ✅What are the first signs of being gluten intolerant?
- 🫢What are uncommon symptoms of gluten sensitivity?
- 🤯What can be mistaken for gluten intolerance?
- ❓How to test for gluten intolerance
- 🚫Rule Out Celiac Disease
- 🚫Cut Out Gluten from Your Diet
- ❣️Treatment for Gluten Intolerance
- ✅Prevention of gluten intolerance symptoms
- 🔄What's the difference between gluten intolerance and celiac disease?
- 🔄Can you go from gluten intolerance to celiac disease?
- 🍑Bottom Line on Gluten Intolerance Symptoms
- Want more?
- 📚More resources to check out
- 💬 Comments
Sometimes it's called Non-Celiac Wheat Sensitivity (NCWS), Gluten Sensitivity (GS), or Gluten Intolerance (GI).
But they're all basically the same thing: different names for gluten intolerance.
🍞What is gluten?
Gluten is a mixture of proteins found in wheat, barley and rye. It's the part of the grain that gives bread it's structure and pull-apart ability.
Gluten is pretty common in the typical North American diet.
So when you think about what you typically eat, there's a good chance you eat foods containing gluten at most meals.
Here's a list of the main sources of gluten for a lot of people:
- Bagels
- Bread
- Cake
- Cereals
- Cookies
- Crackers
- Muffins
- Oats - with an exception: you can buy certified gluten-free oats (regular oats can contain wheat from cross contamination in the field they’re grown in)
- Pancakes
- Pasta
- Tortillas
- Waffles
But there's one catch to the list above - it's not a complete list.
Gluten can be hiding in sooo many places you might not think about. Beer, chicken broth, candy, chips - even soy sauce - can be sources of gluten.
Be sure to grab this cheat sheet so you know where to cut out the gluten today. And read those labels on products to be sure.
🗺️How common is gluten intolerance?
Gluten intolerance is becoming more and more common all over the world.
It has a prevalence of about 0.5% - 13% worldwide and is more common in women(1).
So yah, it's pretty common when you think about it!
But you know one of the worst parts of this? You could go years without a correct diagnosis and end up suffering - when you don't have to!
There's so many unanswered questions about gluten intolerance - especially the symptoms of gluten intolerance.
This is a huge problem for so many of us!
This can mean you're doing things that you don't NEED to do, like:
- Taking medications that aren't right for you
- Restricting your diet in ways that are inconvenient and just not fun
- Missing out on experiences with friends and family because you can't get your symptoms under control
At worse, these can be downright harmful and at best, they waste your money and your time🙅♀️
I should know because I wasted so much time, energy, money AND took meds I didn't need to. This was my experience for years before I was diagnosed.

✅Signs and Symptoms of gluten intolerance
There's so many different signs and symptoms of gluten intolerance.
It's likely that you'll have symptoms that are specific to your body too. No one person is exactly that same as the next person.
Which means that it's very hard to diagnosis gluten intolerance on symptoms alone because person to person, the symptoms of gluten intolerance are so different.
Not only can the actual symptom(s) of gluten intolerance differ person to person but the SEVERITY of the symptom can too (ie, how bad it is.)
Symptoms of gluten intolerance involve intestinal and "extra-intestinal" symptoms.
- Intestinal symptoms refer to symptoms that are "of or in" the intestine. An example would be bloating or diarrhea.
- "Extra-intestinal" refers to "outside" the intestine, ie symptoms that don't involve the intestinal tract. Example of these can be join pain, fatigue or "brain fog".
🙋♀️Some of the most common symptoms of gluten intolerance
- Anxiety
- Ataxia
- Abdominal pain
- Bloating - sometimes called "gluten bloat"
- Constipation
- Stomach pain
- GERD (Gastric Esophageal Reflux Disease) or reflux
- Depression
- Diarrhea and sometimes frequent diarrhea
- Extra-intestinal manifestations such as canker sores and chronic skin conditions like, dermatitis herpetiformis
- Fatigue
- Inability to concentrate on work
- Inability to memorize various things
- Indigestion (also called "dyspepsia")
- Join pain
- Nausea
- Non-specific symptoms including "brain fog"
- Regular headaches
📝Grab the Gluten Intolerance Symptom Checklist
Gluten Intolerance Symptom Checklist (PDF)
✅What are the first signs of being gluten intolerant?
Like a lot of conditions, signs and symptoms of being gluten intolerant will vary person to person.
In general though, here are some early signs to look out for:
- Digestive Problems: A classic sign is digestive discomfort after consuming gluten-containing foods. Look out for bloating, gas, abdominal pain, or even diarrhea after eating things like bread, pasta, or cereal.
- Fatigue and Brain Fog: Feeling unusually tired and foggy after eating gluten-heavy meals could be a sign. Some people experience a sort of mental cloudiness after consuming gluten.
- Headaches: Regular headaches or migraines might have a connection to gluten intolerance for some people. Keep track if they tend to occur after you've had gluten-containing foods.
- Joint Pain: Gluten intolerance can sometimes lead to joint pain or stiffness, resembling symptoms of arthritis.
- Skin Issues: Skin problems like eczema, rashes, or a condition called dermatitis herpetiformis (itchy, blistering skin rash) might pop up due to gluten intolerance.
- Mood Swings: Some individuals experience mood shifts like anxiety, depression, or irritability as a response to gluten intake.
- Digestive Irregularities: Beyond diarrhea, constipation might also be a sign. If your digestive system seems a bit out of whack, gluten intolerance could be at play.
- Unintended Weight Changes: Sudden weight loss or gain without any major changes to your diet or activity level might be linked to gluten intolerance.
If you're concerned about any symptom or sign, talk to a trusted health care provider.

🫢What are uncommon symptoms of gluten sensitivity?
- Neurological Symptoms: Gluten sensitivity can sometimes mess with your nervous system. Keep an eye out for things like tingling sensations, numbness, or even unexplained coordination issues.
- Balance and Coordination Problems: Speaking of coordination, some individuals might experience issues with balance and coordination that seem unrelated to gluten but could actually be connected.
- Dental Issues: Yep, teeth can be gluten-sensitive too. Some people report tooth enamel defects, canker sores, or even frequent cavities as potential markers of gluten sensitivity.
- Migrating Joint Pain: If your joint pain shifts around from one joint to another and seems a bit mysterious, gluten might be playing a sneaky role.
- Aphthous Ulcers: These are those pesky little mouth ulcers that pop up out of nowhere. They might be an uncommon clue to gluten sensitivity.
- Chronic Fatigue: While fatigue isn't uncommon, chronic fatigue that doesn't improve with rest might be an indicator. It's not just about feeling tired; it's more like an ongoing exhaustion.
- Fibromyalgia-like Symptoms: Some people with gluten sensitivity experience symptoms similar to fibromyalgia, including muscle pain, tender points, and fatigue.
- Depression and Anxiety: These mental health symptoms might be unexpected signs of gluten sensitivity. Keep track if they seem linked to gluten intake.
- Autoimmune Issues: Gluten sensitivity might trigger or exacerbate autoimmune conditions, causing a range of symptoms that might not immediately point to gluten.
- Gastrointestinal Bypass: Unlike the typical bloating and diarrhea, some gluten-sensitive individuals might experience symptoms like nausea, vomiting, or even acid reflux.

🤯What can be mistaken for gluten intolerance?
Gluten intolerance can look like a few different conditions.
It can really make your head spin! Is the problem gluten? Maybe dairy? Or menopause? Candida? An undiagnosed medical issue??
Frustrating, definitely. Here's a list of conditions that show up in very similar ways to gluten intolerance:
- Irritable Bowel Syndrome (IBS): The symptoms of IBS can be pretty similar to those of gluten intolerance – think bloating, abdominal pain, and changes in bowel habits. It can sometimes be VERY challenging to tell the difference between the two.
- Wheat Allergy: This one's a bit of a chameleon. A wheat allergy can share symptoms with gluten sensitivity, but it's an allergic response to proteins in wheat, not specifically gluten.
- Lactose Intolerance: Lactose intolerance often brings bloating, gas, and stomach discomfort – just like gluten intolerance. The overlap can be confusing, so it's worth considering both possibilities.
- Other Food Intolerances: Sometimes, it's not just gluten causing the problem. Other food intolerances, like to dairy, fructose, or even FODMAPs, can mimic the symptoms of gluten sensitivity.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis can show up with symptoms that might be mistaken for gluten intolerance, like diarrhea, abdominal pain, and fatigue.
- Celiac Disease: Wait, what? Yes, celiac disease itself might masquerade as gluten intolerance. Celiac disease is an autoimmune disorder triggered by gluten, but its symptoms can be all over the map.
- Sensitivity to Other Grains: While gluten is a protein found in wheat, barley, and rye, some folks might actually be sensitive to other grains like oats or corn, causing similar symptoms.
- Stress and Anxiety: Sometimes, emotional stress or anxiety can cause digestive symptoms that might be mistaken for gluten sensitivity.
- Other Health Conditions: Conditions like thyroid disorders or hormonal imbalances can mess with your digestion and cause symptoms similar to gluten intolerance.
- Normal Variability: Keep in mind, everyone's digestive system has its quirks. What might seem like gluten intolerance could actually just be a response to certain foods that your body isn't a huge fan of.

❓How to test for gluten intolerance
At the time of writing this, there isn't a straight-forward test for gluten intoelrance.
Recent studies show that the accurate diagnosis of gluten intolerance is complicated at best.
Gluten intolerance may be immune-related but there is currently no diagnostic test from a reliable biomarker (1, 2).
Unlike celiac disease where the gold standard way to get a definitive diagnosis is a biopsy of the small intestine while consuming a gluten-containing diet, there's no real test for gluten intolerance (1,2).
Not only that, but there’s a lot of overlap in symptoms between gluten intolerance and other gastrointestinal and digestive disorders. This makes getting a clear diagnosis even more difficult.
Plus, here's the kicker: you can have gluten intolerance and not have celiac disease or wheat allergy(2).

Combine all this with the fact that the pathophysiology of gluten intolerance is largely unclear, including what triggers this condition and all of this can make it really tough to figure out what's the cause of the non-specific digestive symptoms.
Now there is one way to test for gluten intolerance from the research:
- You basically cut out gluten for some time and then watch for any symptoms after you start eating gluten again. Also known as an "elimination diet"
For example, Catassi et al (2015) recommend a double blind placebo controlled gluten challenge, including a one-week challenge followed by a one-week wash-out of strict gluten-free diet and a new crossover to the second one-week challenge (2).
This might be the most reliable procedure so far for diagnosing gluten intolerance but it doesn't really work for "real life."
Great for clinical trials, but hello?
With your busy life, going from work to kid pick-ups to making suppers and lunches and never-ending(!) snacks in between, it's too much to even think about.
You don't have time for clinical-trial-like protocols here. You still have to live.
So. What to do?
🚫Rule Out Celiac Disease
We know you can't rely on symptoms alone to tell the difference between celiac disease and gluten intolerance.
And that's because both gluten intolerance and celiac disease can cause similar symptoms in you.
So the first step to figuring out if what you have is gluten intolerance is to test for celiac disease.
Most if not all of the published research to date recommends that gluten intolerance be diagnosed after ruling out celiac disease.
If you want to go this way, talk to your health care provider who can get things started for you.

🚫Cut Out Gluten from Your Diet
But what if you don't want to wait to get tested?
If you're like me and want relief from your symptoms like yesterday, you don't have to wait to get a blood test and / or a biopsy of your small intestine.
There's another option.
Many clinicians will recommend an “open gluten challenge”, which is what my gastroenterologist recommended.
This is really the most practical way to do it: you simply cut out gluten for 2 weeks and see if your symptoms improve.
This way is of course, based on your ability to follow a gluten-free diet.
For me, I was pretty wishy-washy with the gluten-free diet until I made it stick.
For good.
Do NOT go gluten-free alone. Join me to get all the gluten-free recipes or get support from a trusted healthcare provider.

If you want to know more about out how I finally cut the gluten, check out: How to Get Rid of Gluten Bloat (Fast!)
❣️Treatment for Gluten Intolerance
The treatment for gluten intolerance is a gluten-free diet.
For me, going gluten free was the only way I could:
- Come off all my medications for reflux
- Get rid of my daily, debilitating nausea
- End my embarrassing burping
- And never have a severely bloated stomach again🥳
This was my own personal experience and yours might be different so always check with a trusted healthcare provider before making drastic changes to your lifestyle, especially when it comes to medication.
But choosing a healthier diet and one that's gluten-free is something you can do right now.
And be sure you're signed up for email updates so you get the weekly emails from me.
We're on this journey to a completely gluten-free lifestyle together!
✅Prevention of gluten intolerance symptoms
At the time of writing, the "prevention" part of gluten intolerance is focused around preventing the symptoms of gluten intolerance.
Which really goes hand-in-hand with the treatment: stopping the effects of eating gluten before they even start.
What would be even better is to prevent the intolerance in the first place!
But like other health conditions with an unclear cause: you can't truly prevent something if you don't know the cause.
And as for where we are right now, the mechanism or "cause" of gluten intolerance remains a mystery.
In their review article, Casella et al (2018) discuss, among other things, that progress is being made in starting to uncover some of the mechanisms behind the symptoms for people with gluten intolerance.

For example, in a case report by Rostami et al (2015), the researchers discuss how the blanket diagnosis of Irritable Bowel Syndrome (IBS) in patients with symptoms like dyspepsia (or indigestion), constipation or diarrhea, doesn't address a gluten (or lactose) intolerance caused by an infection in the gut.
The site of infection can produce different symptoms. For example, if the virus or bacteria was present in the small bowel or colon then IBS-like symptoms were more likely.
If the infection was in the stomach or duodenum (the first part of the small intestine), then functional dyspepsia (indigestion) was more likely.
("Dyspepsia" is just a fancy name for indigestion. And isn't actually a symptom itself but refers to pain or discomfort in the upper abdomen that happens after eating. Symptoms of dyspepsia include bloating, discomfort, pain, nausea, feeling too full and gas.)
In these cases, the researchers note that the symptoms that point to an IBS diagnosis, are actually covering up a gluten sensitivity.
As a result, the patient doesn't get the right treatment (ie, they don't get support with a gluten-free diet.)
More research is ongoing to try and figure out the cause of gluten intolerance and get easier and more specific ways to help clinicians diagnosis it in their patients.

🔄What's the difference between gluten intolerance and celiac disease?
Gluten intolerance and celiac disease are very different conditions.
Gluten intolerance (and the whole spectrum of gluten-related disorders) is probably more complicated than we know right now.
In many ways, we're just scratching the surface in trying to better understand this condition that is becoming more and more common.
We're still trying to:
- Get a reliable biomarker or easy diagnostic test for gluten intolerance
- Figure out the different types of symptoms in people that happen after they eat of gluten and,
- Learn what types of individual factors play a role in the severity of gluten sensitivities in general

Celiac disease, on the other hand, is an autoimmune disease where gluten causes damage to the lining of the intestine. Diarrhea, stomach pain and bloating are very common in celiac disease.
In extreme cases, celiac disease can cause nutrient deficiencies, malabsorption disorders, and cause people to become very sick.
On the plus side, celiac disease has well-defined and well agreed upon diagnosis criteria, clear treatment protocols, and is generally a well-accepted condition by the public.
So although celiac disease and gluten intolerance are related by the common thread of the ingestion of gluten triggering symptoms, they're very different conditions.
- For example, if you have gluten intolerance but not celiac disease, you won't get the same intestinal damage that people with celiac disease get.
- And you won't test positive for celiac disease or wheat allergy with an intestinal biopsy.
As more research is done in the area of gluten-related disorders, personally, I really hope that a reliable way to test for gluten intolerance is found.
So many people are mis-diagnosed by well-meaning health care professionals as having IBS or simple GERD (like I was), and go through years of discomfort and pain, trying to figure out what the heck is causing their symptoms and what to do about it.
I spent years in pain, discomfort and confusion too.

Not to mention, taking medications that weren't helping.
Going gluten-free helped me get control back to my eating, my health and my life.
If you think you have a sensitivity to gluten and are ready to find relief like I was, get started going gluten-free today.
Don't wait like I did!
Start with this list of Foods to Avoid for Gluten Intolerance so that you can get the majority of gluten out of your diet ASAP.
🔄Can you go from gluten intolerance to celiac disease?
There is no definitive answer for this question but it has been shown that people can have one (or more) gluten-related disorders.
This could mean that someone could have gluten intolerance and then be diagnosed with celiac disease.
However, because celiac disease involves the activation of the immune system and the damage to the lining of the intestine, which gluten intolerance does not, the only way to know for sure, is the biopsy of the small intestine.
Again, because there is no easy and straight-forward way to diagnosis gluten intolerance, it's recommended to first rule out celiac disease and then base the diagnosis on the symptoms.
🍑Bottom Line on Gluten Intolerance Symptoms
If you think you might have celiac disease or gluten intolerance, talk to your doctor.
If you want to start on a gluten-free diet now to start feeling better, I have good news for you!
You can start here:
CHEAT SHEET: foods to avoid with gluten intolerance
Getting tested for celiac disease - and finding out that I didn't have it - was the thing that finally put me on the path to feeling better.
Going gluten-free for life and eating healthy is possible.
Get in on my weekly email updates so that you get all the healthy and gluten-free recipes from me and you don't miss a thing.
I'll see you on the inside🙋♀️
Want more?
Sign-up to get all the healthy and gluten-free recipes delivered straight to your inbox each week.
"*" indicates required fields
~April
📚More resources to check out
References:
1. Asri N, Rostami-Nejad M, Anderson RP, Rostami K. The Gluten Gene: Unlocking the Understanding of Gluten Sensitivity and Intolerance. Appl Clin Genet. 2021;14:37-50. https://doi.org/10.2147/TACG.S276596
2. Catassi C, Elli L, Bonaz B, Bouma G, Carroccio A, Castillejo G, Cellier C, Cristofori F, De Magistris L, Dolinsek J, Dieterich W, Francavilla R, Hadjivassiliou M, Holtmeier W, Körner U, Leffler DA, Lundin KEA, Mazzarella G, Mulder CJ, Pellegrini N, Rostami K, Sanders D, Skodje GI, Schuppan D, Ullrich R, Volta U, Williams M, Zevallos VF, Zopf Y, Fasano A. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients. 2015; 7(6):4966-4977 (downloaded)
3. Casella G, Villanacci V, Di Bella C, Bassotti G, Bold J, Rostami K. Non celiac gluten sensitivity and diagnostic challenges. Gastroenterol Hepatol Bed Bench 2018;11(3):197-202).
4. Rostami K, Rostami-Nejad M, Al Dulaimi D. Post gastroenteritis gluten intolerance. Gastroenterol Hepatol Bed Bench. 2015;8(1):66-70.
5. Meijer C, Shamir R, Szajewska H, Mearin L. Celiac Disease Prevention. Front Pediatr. 2018;6:368. Published 2018 Nov 30. doi:10.3389/fped.2018.00368
6. Leonard MM, Sapone A, Catassi C, Fasano A. Celiac Disease and Nonceliac Gluten Sensitivity: A Review. JAMA. 2017 Aug 15;318(7):647-656. doi: 10.1001/jama.2017.9730. PMID: 28810029.





Comments
No Comments